
By John Kitchens, MD
Choroidal detachment infrequently occurs following glaucoma filtering surgery. This post-operative complication can be of either the serous or hemorrhagic variety. Serous choroidal detachments will often resolve with conservative management. Choroidal detachments are approached surgically if they are appositional or if they are large and do not demonstrate resolution with conservative management.
The drainage procedure involves placing and infusion line in through the pars plana or in the anterior segment if the detachment prevents safe placement of the line posteriorly. A scleral cut-down is performed in the area of the most prominent detachment. Typically, a serous choroidal detachment will drain effectively in this manner. Hemorrhagic detachments often require a period 10 to 14 days to allow the hemorrhage to “liquify” prior to drainage.
Our approach involves the use of the Alcon 25-gauge instrumentation to allow for drainage of a serous choroidal detachment. The advantages of this approach include: a self-sealing incision, minimal conjunctival manipulation, and a more complete drainage than with previous techniques.
Case:
A 72 year old gentleman had undergone trabeculectomy surgery one month prior. The initial two postoperative weeks after his glaucoma surgery were complicated by ocular hypotony and progressive choroidal detachments. On the third week, he was referred for evaluation and treatment. On initial examination, his visual acuity was hand motions and his intraocular pressure was 10. He had large choroidal detachments that were appositional in nature (see figures 1 and 2 from surgical video). Due to the fact that the patient was on anticoagulation therapy, his surgery was scheduled for one week from his initial visit.
Technique:

Figure 1. External view demonstrates the large serous choroidal detachments.

Figure 2. Internal view through the Biom viewing system shows large choroidal detachments.

Figure 3. An chandelier light was placed inferiorly to allow for adequate visualization of the posterior segment. A standard Alcon 25 gauge cannula was utilized inferonasal where the choroidal detachment was least prominent. Note that the infusion cannula is placed more anteriorly (~2mm from the limbus) in an attempt to avoid the choroidal detachment.

Figure 4. The standard cannula is trimmed to a length of approximately 2mm to minimize the potential for iatrogenic trauma when the detachment is drained.

Figure 5. The cannula is replaced onto the trocar.

Figure 6. The trocar/cannula is introduced into the suprachoroidal space in the area of the most prominent detachment approximately 8 to 10 mm posterior to the limbus.

Figure 7a. The trocar/cannula is advanced at an angle into the suprachoroidal space.

Figure 7. The cannula allows for rapid drainage of the suprachoroidal fluid.
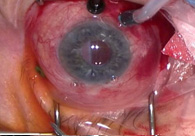
Figure 8. The cannula allows for rapid drainage of the suprachoroidal fluid.

Figure 9. The cannula is removed.

Figure 10. The sclerotomy has sealed.

Figure 11. Intraoperative photo shows a marked resolution of the choroidal detachment with the posterior pole visible.
Have a question or comment on this article? Use the “Comment” link above to leave your thoughts, and the author will respond.