Retinal imaging has evolved through many years. However, there are certain sentinel landmarks which have changed the way we view and understand the retina forever. The earliest of these occurred 400 years B.C. when Democritus first proposed the construction of the eye as a hollow tube connected to the brain (
figure 1). Four hundred years later Celsus advanced the understanding of the ocular system to include a lens, the anterior chamber, and a vitreous (
figure 2). No one can question the importance of these contributions in the understanding of ocular imaging.
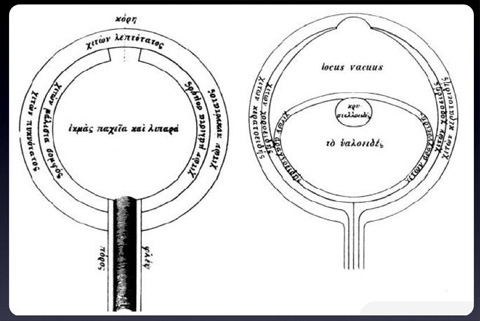
Figure 1. Illustrations by Democritus (400 BC) on the left and Celsus on the right (from Duke-Elder, 1961).

Figure 2. Timeline of modern retinal imaging.
Fast forward 1800 years later, this is what I would consider the modern era of retinal imaging. No one can question the contribution of Helmholz to ophthalmology with the advent of the direct ophthalmoscope in 1851. Certainly, this is as much of a landmark in medicine as it is in ophthalmology. Modern imaging of the retina began in 1886 with Jackman and Webster who produced the first human retinal photographs in vivo. Many other contributions were made over the next 50+ years until two medical students (Novotny and Davis) at Indiana University performed the first fluorescein angiogram in 1961. Since that time, angiography has become a mainstay in the diagnosis and management of retinal diseases including macular degeneration, diabetic retinopathy, and retinal vascular occlusions just to name a few.
The basic technique of fluorescein angiography has remained relatively unchanged since reported in 1961. Advances in image capture technology have been improved drastically. One major advance occurred in the mid-80s with the development of digital photography. The ability to perform digital angiography did not become widely accepted until the mid to late 90s but since that time has become ubiquitous among retinal specialists.
The advent of OCT in 1991 also caused a paradigm shift in retinal imaging. Optical coherence tomography (OCT) allowed a noninvasive way of diagnosing and managing ocular conditions that was more quantitative, faster, and required fewer resources than angiography. In history, OCT may well rival Helmholz’s ophthalmoscope in its contribution to our understanding and treatment of retinal disease. Certainly, it is the single most utilized diagnostic test performed by retina specialists. One major difference between angiography and OCT technology is that OCT technology continues to evolve at a rapid pace.
Currently, there are very few ways to image the peripheral retina during an angiogram. One way involves creating a montage image during the angiogram process. Several images throughout the angiogram are obtained utilizing a standard camera. These 30 or 50 degree images are then montaged together by special imaging software. This creates a more complete view of what’s going on spatially. Unfortunately, the montage image shows various phases of the angiogram making it less useful to interpret what’s occurring throughout — early phase photos may be right next to late phase photos creating confusion (figure 3). In addition, the montage system is still limited on how peripheral images can be obtained. It is also very photographer dependent. Another possible method of obtaining widefield images is with a Staurenghi lens system. This lens system provides unbelievable images but is very difficult to use and it requires an extremely skilled photographer and cooperative patient. Two other systems can provide widefield photography: the Retcam imaging system (used primarily in pediatric retina for ROP management) and the Panoret system. Both of these systems provide 130 degree images of the retina with a contact system. The disadvantages of these systems include their image resolution, the fact that they require ocular contact for image acquisition, and the fact that they require a fairly skilled photographer to obtain the pictures.

Figure 3. Montage angiogram of serpiginous choroiditis.
A Major Shift…
A major shift in wide field imaging and angiography is about to occur with the Optos imaging system. Optos has already developed a non-mydriatic camera system that is used in optometry offices for screening examinations and documentation. Over the past few years they have developed a much more refined retina specific imaging system called the Optomap FA. This system allows for the capture of high-resolution (3000 x 3000 pixels), widefield (200 degree) retinal photographs and angiograms (figure 4). We have been fortunate to trial the system in our office over the past few months and I must say that I’ve seen things that are fairly remarkable. Although the majority of what we concern ourselves with involves the macular area, there are a variety of fascinating things that occur in the peripheral retina in conditions like diabetic retinopathy, retinal vascular occlusions, and inflammatory conditions.

Figure 4. Optos widefield angiogram of a normal retina.
Diabetic Retinopathy
One of the things that shocked me when imaging diabetics with this widefield technology is the degree of peripheral non-perfusion found in some patients. Both the DRS and ETDRS did a very good job of establishing certain risk characteristics associated with progression of diabetic retinopathy. However, I have seen patients that I would classify as moderate to severe non-proliferative diabetics that have profound peripheral non-perfusion on angiography. I’ve also seen other patients in a similar classification that have excellent peripheral perfusion. There have also been cases of what appears to be asymmetric retinopathy with a vitreous hemorrhage in one eye and what appears to be more profound nonperfusion in the fellow eye (figure 5). It is possible that these widefield images may allow us to better understand and classify diabetic retinopathy. These images may also allow us to focus our treatment (PRP) to specific areas of non-perfusion and decrease the iatrogenic visual field loss that can be associated with laser treatment. I’ve certainly learned that there is a lot more non-perfusion than I ever expected to be occurring in diabetic patients. This imaging process may also explain why some patients have recurrent CSDME that responds more favorably to anti-VEGF therapy by identifying extensive areas of non-perfusion which may result in increased VEGF production stimulating macular leakage (figure 6). It has been theorized that PRP to the areas of nonperfusion may reduce the VEGF-mediated leakage and ultimately decrease the number of treatments (injections) that may be required for these individuals.

Figure 5a. Left eye of a patient with vitreous hemorrhage from PDR.

Figure 5b. Right eye of the same patient shows worse perfusion and more neovascularization.

Figure 6. Patient with profound peripheral nonperfusion and recurrent CSDME that is responsive to Avastin.
Venous Occlusive Disease
The CVO study utilized angiography to determine the perfusion status (ischemic or nonischemic) of a vein occlusion. Unfortunately, they are imaging techniques or typically only of the posterior pole and surrounding retina — they missed a tremendous amount for a full retina. This system can provide for a complete evaluation of the peripheral and macular non-perfusion allowing us to better classify these occlusions early on. I’ve also been astounded by our images obtained in branch main occlusions. You get a much richer understanding of the degree and affect of what appears to be a limited BRVO when you actually can see peripherally and understand a more far-reaching impact of these inclusions (figure 7).

Figure 7. Patient with superotemporal BRVO. Interestingly, the patient’s vision is 20/20.
AMD
Benefits in the management of AMD with widefield imaging? Yes, I believe there may be a benefit in using this technology in patients with AMD. One reason is that peripheral changes can give insight into the overall condition of the RPE. Some studies have suggested the association of the complement factor H variant with more diffuse, global, peripheral changes (as opposed to the LOC387715 mutation which these same authors have suggested to have a more macula-specific phenotype). Widefield images may help with classifying risk factors for AMD progression. It should also be noted that the addition of autofluorescence is planned for the Optomap FA in the future. This addition would allow for a different understanding of the various peripheral changes that we currently “gloss over” in these patients.
Other Areas
A variety of other areas including ocular inflammatory diseases, genetic diseases, trauma, and retinal detachments can be imaged with this system. The widefield nature can give a more complete understanding of many of these conditions and allow for improved diagnosis, patient understanding and management. One obvious area that I have not emphasized is the evaluation and management of ocular tumors. This technology will be a “must have” for anyone who manages ocular tumors on a regular basis.
The Drawbacks
Being an early evaluator of the system I can tell you that there are certain drawbacks. The color images have a “greenish hue” to them and are frankly not as good from a color standpoint as a regular fundus camera. Also, there are still issues with eyelash artifacts that are particularly bothersome in the inferior field of the images (caused by the superior eyelid). Because of the design of the system, it is difficult to hold open the patient’s eyelid and still get a good image. Finally, it certainly takes some time for a photographer to get used to this new system. They are not sitting across from the patient and they cannot focus the camera on the retina prior to taking the picture. Even though photographers have no idea where they are aiming, the camera’s excellent auto focus almost always takes pictures that are in good focus.
What They Have Done Well
Aside from the ability to obtain quality widefield high resolution angiograms, Optos has delivered a very robust and mature software program. Their Windows®-based interface works seamlessly with the camera. The software package allows for measurement of lesions and cup-to-disc ratio. It also allows for labeling and drawing areas on the images. The most unique aspect of the viewing software is the ability to place a 3-D model of the eye around the image. This feature provides an improved way to explain the disease process to the patient.
Summary
All things considered, this technology is fascinating. It is certainly not as revolutionary and practice changing as the OCT, but it certainly will provide more understanding to various conditions that involve the peripheral retina. A few improvements need to be made (better color images, decreased artifacts), but it is impressive. The current imaging technologies are just the tip of the iceberg. This device, and others like it, will allow us to better understand and treat retinal conditions.
Disclosures:
Dr. Kitchens has no financial interest in Optos. His practice, Retina Associates of Kentucky, did receive the Optomap FA unit as a beta testing site for this new technology.
Have a question or comment on this article? Use the “Comment” link below to leave your thoughts, and the author will respond.